C3 - 04: SURGICAL INFORMED CONSENT PERCEPTIONS IN SUDAN: POTENTIAL FOR IMPROVEMENT THROUGH TRAINING AND EDUCATION
Natasha Abadilla, BA1, Ahmed ElSayed, MD2, Sherry Wren, MD, FACS, FCS, ECSA1; 1Stanford School of Medicine, 2Alzaiem Alazhari University
Introduction: It is a legal requirement in the US to obtain informed consent – the discussion of potential risks and benefits between a doctor and patient – prior to an invasive procedure; however, informed consent policies in low resource countries may not be defined, enforced, or culturally acceptable. Sudan, a lower middle income country, has a national policy on informed consent, but its application has not been studied. This project assesses perceptions of informed consent from physicians and patients to determine current practice and inform training to improve patient understanding of their surgical procedures, as well as perceptions of patient rights and autonomy.
Methods: Survey instruments (English and Arabic) were administered to post-operative surgical patients and surgical service physicians in 3 public hospitals in Khartoum. Focus groups with randomly selected physicians and surgical patients were done to expand survey themes. Data was collected by trained data collectors in July 2017.
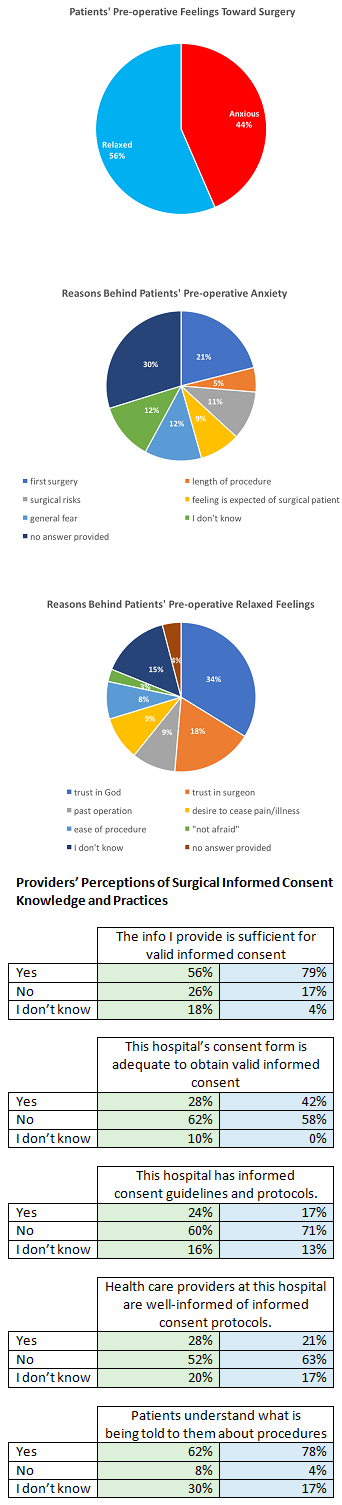
Preliminary Results: Data was gathered from 136 surgical patients, 50 trainees and 24 attending surgeons. Overall 72% of trainees and 58% of attendings were not aware of their hospitals’ informed consent protocols. The majority of both groups 76% (trainees) and 84% (attendings) stated that in general health care providers were not well-informed of protocols. Post-operatively 57% of patients reported they would have wanted more information about their procedure before it was done, and 61% said that more information would have made them less anxious about their procedures. The predominant reason patients feel at ease before surgical procedures was found to be the patients’ “trust in God.” Focus group data revealed discontent and confusion about informed consent protocols from both providers and patients, and providers’ perceptions that too much information may cause a patient to not desire a procedure.
Conclusions: There is a knowledge deficit of national policies as well as a disconnect regarding the amount of information providers believe is appropriate to give a patient for valid informed consent and the amount of information patients desire before a surgical procedure. This study uncovers opposing perceptions and reveals potential for improved training for physicians in Sudan.
