PS1 - 02: USE OF NON-TECHNICAL SKILLS CAN PREDICT MEDICAL STUDENT PERFORMANCE IN ACUTE CARE SIMULATED SCENARIOS
Jackie S Cha, MSE1, Nicholas E Anton, MS2, Tomoko Mizota, MD2, Julie M Hennings, MSN, RN, CCRN2, Megan A Rendina, BS2, Katie Stanton-Maxey, MD2, Hadley E Ritter, MD2, Dimitrios Stefanidis, MD, PhD2, Denny Yu, PhD1; 1Purdue University, 2Indiana University School of Medicine
Introduction: Physician non-technical (NT) skills are critical to patient care, but emphasis and evaluation of these skills are limited in current medical education. Validated rating scales have been developed to assess NT skills such as the Oxford non-technical skills scale (NOTECHS) which evaluate constructs such as communication and decision making. The objective of this study was to determine if medical student clinical performance during a simulated acute care scenario (ACS) can be predicted using an adapted NOTECHS scale.
Methods: Twenty-seven medical students participated in ACS. Each scenario lasted for 10 minutes and was facilitated by a nurse confederate who evaluated student clinical performance on a standardized checklist. Scenarios were video recorded, and the students’ NT skills were assessed using an adapted NOTECHS tool developed by a team of clinicians, nurses, and human factors (HF) engineers. The constructs of communication, situation awareness (SA), cooperation, leadership, and decision making were rated between 0-6, where 0 represented very problematic behavior which endangered patient safety (e.g., ignoring support from team) and 6 represented model behavior (e.g., encourages vigilance). Final average performance was calculated. All student NT skills were evaluated independently by three trained HF and clinical raters, and the students’ clinical performance was evaluated by an experienced nurse confederate. Linear regressions predicting clinical performance using NT constructs were conducted on SPSS.
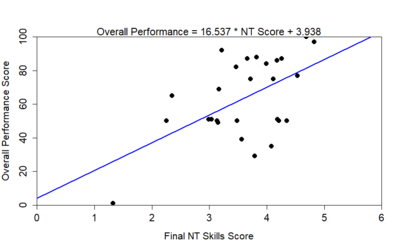
Results: It was found that final NT skills score significantly predicted the student’s overall clinical performance in the scenario (p=0.003, r2=0.302; Figure 1). Each of the individual NT constructs also significantly predicted performance: communication (p=0.020, r2=0.199), SA (p<0.001, r2=0.450), cooperation (p=0.031, r2=0.172), leadership (p=0.006, r2=0.266), and decision making (p=0.010, r2=0.239).
Conclusions: Medical student NT skills can significantly predict clinical performance during ACS. SA was a better predictor of performance than the final NT score and other individual constructs, which suggests that monitoring, understanding, and anticipating the team and patient are critical in successful performance in acute care settings. NT assessments provide deeper insight to how these constructs influence performance and can be used to focus training and provide specific feedback to trainees. Additional validation studies for this tool in ACTS is ongoing.
