PS2 - 05: MULTI-CENTER, PROSPECTIVE COHORT STUDY EVALUATING THE IMPLEMENTATION OF A MEDICAL STUDENT HANDOFF CURRICULUM DURING THE SURGERY CLERKSHIP
Rebecca L Hoffman, MD, MSCE1, Afif Kulaylat, MD2, Brian D Saunders, MD2, Steve Allen, MD2, Cary B Aarons, MD1; 1University of Pennsylvania, 2Penn State Hershey School of Medicine
Introduction: Early introduction to essential communication skills, like handoffs, could provide time for deliberate practice for medical students. We sought to determine if implementation of a handoff curriculum would improve students’ knowledge, comfort and experience with patient handoffs during the surgery clerkship.
Methods: A multi-center prospective cohort study was performed during the 2016-2017 academic year at two medical schools. Students were assigned by block to receive handoff training (HO; 2/4 blocks) or not (No-HO; 2/4 blocks). Training consisted of a didactic lecture, video review and practice session. Students completed a knowledge test and survey regarding exposure to handoffs, confidence and anxiety (Likert scale 0-4) prior to the clerkship and immediately following their 4-week general surgery(GS) block. T-tests and chi-squared tests were performed, as appropriate.
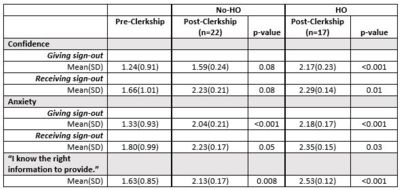
Results: Seventy students completed the pre-clerkship survey(24.1%) and 39(13.4%) completed the post-GS survey; 22 in No-HO, 17 in the HO group. There were no significant differences between institutions pre-clerkship except having previously witnessed a verbal handoff (p=0.01). Mean(SD) knowledge scores did not improve significantly in either group (15.8/20(2.9) pre; No-HO 16.8(2.4), p=0.15; HO 16.5(2.7), p=0.37). Students in the HO group were significantly more involved in creating written sign-outs (52.9% HO vs 18.2% No-HO, p=0.02) and more often gave verbal handoffs (29.4% HO vs 4.6% No-HO, p=0.03). HO students reported more significant improvements in confidence and anxiety regarding giving/receiving handoffs and a more significant increase in understanding the information to provide (Table). Only 4(10.3%) were explicitly given opportunities for handoffs by their residents, and 10(25.6%) sought their own opportunities (6 from HO group).
Conclusions: Surgery clerkship students exposed to formal handoff training were more involved in these practices, and expressed greater improvements in confidence/anxiety and understanding with handoffs. Emphasis on this skill should be provided early in training to develop a safer patient care environment.