PS2 - 06: ACS/ASE MEDICAL STUDENT SIMULATION-BASED SURGICAL SKILLS CURRICULUM: ALIGNMENT WITH ENTRUSTABLE PROFESSIONAL ACTIVITIES
Susan Steinemann, MD1, Aimee Gardner, PhD2, Tess Aulet3, Shimae Fitzgibbons4, Andre Campbell5, Robert Acton6; 1University of Hawaii, 2Baylor College of Medicine, 3University of Vermont Medical Center, 4Georgetown University, 5University of California, San Francisco, 6University of Minnesota
INTRODUCTION: The American Association of Medical Colleges’ (AAMC) Entrustable Professional Activities (EPAs) describe the responsibilities to be independently performed by graduating medical students. However, the burden of determining how and when EPAs are taught and assessed is left to each institution. The goal of this study is to examine the extent to which the American College of Surgeons/Association for Surgical Education Medical Student Simulation-based Surgical Skills Curriculum (ACS/ASE Curriculum) can be used by leaders in medical education to fill the EPA teaching and assessment gap. Moreover, we sought to identify barriers to curriculum implementation.
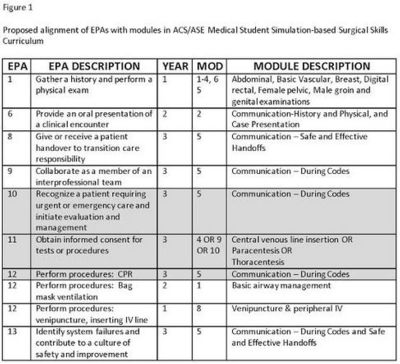
METHODS: A “crosswalk” between ACS/ASE Curriculum modules and the EPAs was created by consensus of the authors. (Figure 1) Senior medical educators were recruited to participate in a Delphi study. The survey contained Likert-type questions regarding conceptual alignment and feasibility of using the ACS/ASE Curriculum for teaching and assessing EPAs. Round 1 included open response questions regarding skills training and “trustable” learners. Additional rounds were conducted until >75% consensus was achieved on the ability of each module to teach or assess an EPA.
RESULTS: Twenty-eight medical educators participated: 10 Deans/Associate Deans, 4 Chairs/Vice Chairs of Education, 9 Clerkship Directors, 3 Simulation Center Directors, 2 Program Directors/Associate Program Directors. Specialties included: Surgery, Internal Medicine, Pediatrics, Obstetrics/Gynecology, Family Medicine, and Social Sciences. Six respondents (21%) indicated they currently use the Curriculum, only one tracked EPAs. The most frequently cited obstacles to using the Curriculum were curricular time (25%) and lack of a faculty champion/buy-in (18%).
At the conclusion of Round 1, consensus was achieved that specific Curriculum modules could be used to teach and assess EPAs 1,6,8,9,12 and 13. (Fig.1-unshaded) Round 2 attained consensus that the Curriculum was insufficient to teach/assess EPAs 10,11 and cardiopulmonary resuscitation (EPA12-CPR). (Fig.1-shaded)
CONCLUSION: Medical education leaders from a variety of disciplines strongly agreed that the ACS/ASE Curriculum can be an effective tool for developing and assessing six AAMC EPAs. Two main barriers to implementation of the ACS/ASE Curriculum are time within the medical student curriculum and faculty support. Future work should identify effective strategies for overcoming these barriers when implementing the curriculum.