PS3 - 02: AN EPA-ALIGNED, MASTERY LEARNING SCRUB TRAINING CURRICULUM SIGNIFICANTLY INCREASES MEDICAL STUDENT KNOWLEDGE AND CONFIDENCE IN OPERATING ROOM STERILE TECHNIQUE
Brittany Hasty, MD, Sarah Miller, BS, Sylvia Bereknyei Merrell, DrPH, Edmund Lee, MD, Dana Lin, MD, James Lau, MD, MHPE; Stanford University
Background: In May 2014, the AAMC released the 13 Core Entrustable Professional Activities (EPAs) for Entering Residency. Under EPA #13 the student is to “engage in daily safety habits”. Unique and stringent hand hygiene techniques are necessary during required clerkships such as surgery. Students need to learn how to scrub in for operations and maintain sterile technique. The consequences of breaking sterile technique are costly and directly threaten patient outcomes. To date, there has been no standardized scrub training curriculum targeted to medical students despite that specialties requiring sterile technique encompass over 40% of nationally matched applicants in 2017. Recognizing the need for a standardized curriculum, we created a multi-faceted, EPA-aligned, mastery learning scrub training curriculum.
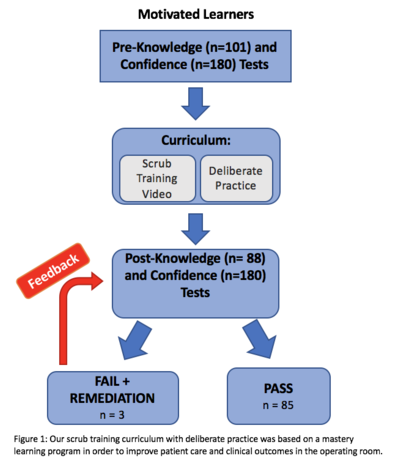
Methods: We assessed for both knowledge and confidence improvements before and after the scrub training curriculum on the mastery learning model (Figure 1). Pre- and post-curriculum data were each analyzed in aggregate, descriptive statistics were calculated, and a paired t-test was performed to identify significant mean differences in self-reported confidence and knowledge scores.
Results: Between April 2017 and October 2017, 101 students completed the pre-knowledge assessment and 88 students completed the post-knowledge assessment. 53% of students identified as female, 61% were in their first year, 70% never scrubbed into an operation, and 60% never received prior scrub training. There was a statistically significant increase in the knowledge assessment score from before (Mean= 66.7%; SD ± 13.2) and following (Mean= 90.1%; SD ± 7.7) the curriculum (p<.001). There was also a statistically significant increase in student confidence of the 180 students who completed both the pre- (Mean= 2.52; SD± 0.84) and post-confidence (Mean= 3.74; SD± 0.75) surveys (p<0.001).
Conclusion: As medical education continues to transition from a time-based model to a competency-based model, novel assessment methods will be required. Here we have demonstrated that a multi-faceted, EPA-aligned, mastery scrub training curriculum increases both student confidence and knowledge of sterile technique. Ultimately, mastery learning and testing are essential to the measurement and achievement of EPAs and provides a springboard toward improving patient care.
