Poster4 - 06: A NOVEL ONLINE EDUCATION MODULE FOR TEACHING THE LYMPH NODE SONOGRAPHIC SCORE
Danielle A Hylton, MSc, John Agzarian, MD, MPH, FRCSC, Yaron Shargall, MD, FRCSC, FCCP, Christian J Finley, MD, FRCSC, Christine Fahim, MSc, PhD, Waël C Hanna, MDCM, MBA, FRCSC; McMaster University
The Lymph Node Sonographic Score (LNSS) uses ultrasonographic features to predict malignancy in mediastinal lymph nodes visualized via endobronchial ultrasound (EBUS). Despite the proven validity of the LNSS, it has not been widely adopted in clinical practice. This may be attributable to the absence of education programs that focus on teaching clinicians how to properly identify endosonographic features. To address this knowledge gap, we developed an online education module to teach clinicians how to interpret ultrasound images using the LNSS.
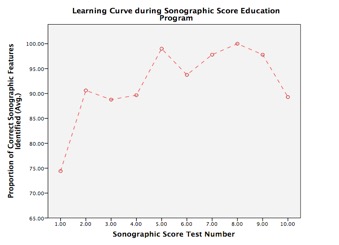
The education module was designed based on spaced-repetition and test-enhanced learning theories. The module was distributed to clinicians in thoracic surgery, general surgery, and respirology. The module included a baseline knowledge assessment, an education component focusing on repetition of concepts, and a post-module assessment to evaluate knowledge acquisition and retention. Efficacy of the program was determined by comparing the percentage of correctly identified endosonographic features as the clinician progressed through the module. Participants were also asked to self-rate their level of confidence in using the LNSS at various points during the module. A learning curve, an analysis of variance (ANOVA), and descriptive statistics were generated.
Fifteen participants (5 residents; 8 fellows; and 2 attending practitioners) completed the education module. A one-way repeated measures ANOVA indicated that the percentage of correctly identified endosonographic features increased significantly as clinicians progressed through the module (p=0.004). This was also indicated by the overall upward slope of the learning curve (Figure 1). After the fourth practice test, proficiency increased on average from a mean of 73.58% (± 2.11%) to 96.58% (± 0.92%) (p<0.001). A dependent samples t-test indicated that the average self-rated confidence with using the LNSS increased significantly as participants progressed through the module (35.85% vs. 57.46%, p=0.011). When asked, 68.40% of participants found the education module helpful and 84.60% would recommend it to others.
Results suggest that this online education module significantly enhances clinician skill and confidence in interpreting the LNSS during EBUS staging of the mediastinum. The evidence provides the foundation needed to test the validity of the education module in clinical settings and to further explore clinician preferences for education programs.