PS1-03: CLINICAL IMPACT OF CRITICAL CARE SUMMER SCHOOL ON JUNIOR RESIDENT CONFIDENCE IN THE SURGICAL INTENSIVE CARE UNIT
Jason Fawley, MD, Ryan Howard, MD, Lena Napolitano, MD; University of Michigan
Purpose: Resident duty-hour limitations with resultant decreased intensive care unit (ICU) rotations have had negative impact on surgical resident education. Junior surgical residents are expected to manage critically ill patients in the surgical ICU with little experience. To address this, we initiated an 8-week course in July/August entitled “Foundations of Critical Care” aka Critical Care Summer School. The course includes independent pre-course preparation, didactic lectures, and simulated management and procedures in critically ill patients. We investigated resident confidence in managing fundamental aspects of critical care and performing common ICU procedures before and after completion of this course.
Methods: After course completion, an anonymous survey was sent to all PGY1 & 2 surgical residents who participated. The survey assessed confidence in performing procedures and managing critically ill patients before and after completing the course. Chi-square analysis was utilized to compare variables. Values are presented as percentage of residents who felt confident before versus after course.
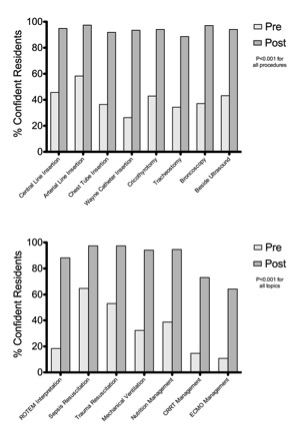
Results: The mean individual session aggregate evaluation for the question “The overall value/quality of this course was high” was 4.47±0.23 (5=strongly agree). The post-course survey response rate was 75.4% (40 of 53) and included 19 females (47.5%). The majority were PGY1 (65%) ages 25-29 (72.5%), and were categorical general surgery residents (32.5%). The course significantly improved resident confidence in multiple ICU procedures, including central line placement (45.7% vs 94.9%, p<0.001), arterial line placement (58.3% vs 97.4%, p<0.001), chest tube insertion (36.4% vs 91.9%, p<0.001), Wayne pneumothorax catheter insertion (26.3% vs 93.5%, p<0.001), cricothyroidotomy (42.9% vs 94.1%, p<0.001), tracheostomy (34.3% vs 88.6%, p<0.001), bronchoscopy (37.1% vs 97.1%, p<0.001), and bedside ultrasound (43.2% vs 94.1%, p<0.001). Regarding clinical knowledge, the course improved confidence in ROTEM interpretation (18.4% vs 88.2%, p<0.001), resuscitation of septic patients (64.7% vs 97.4%, p<0.001), resuscitation of trauma patients (53.7% vs 97.4%, p<0.001), mechanical ventilation (32.3% vs 94.1%, p<0.001), nutrition (38.7% vs 94.6%, p<0.001), continuous renal replacement therapy (14.7% vs 73.1%, p<0.001), and extracorporeal membrane oxygenation (10.8% vs 64.3%, p<0.001).
Conclusions: A junior surgical resident ICU preparatory course was assessed as high quality and value, and was successful in improving resident confidence in critical care.