PS1-08: SURGICAL INSTRUMENT STANDARDIZATION â A PILOT COST CONSCIOUSNESS CURRICULUM FOR SURGERY RESIDENTS.
Kevin Y Pei, Robyn Richmond, Sharmila Dissanaike; Texas Tech University Health Sciences
Introduction: Surgical cost is astronomical in the US and instrument standardization is one potential mechanism for cost savings. While some studies demonstrate cost savings through supply chain management, little is known about surgeon education regarding cost consciousness. Furthermore, there is potential to promote cost consciousness within systems-based practice - an important ACGME core competency among surgical trainees. This study describes a core competency based, multidisciplinary curriculum and evaluates resident attitudes towards operating room equipment standardization.
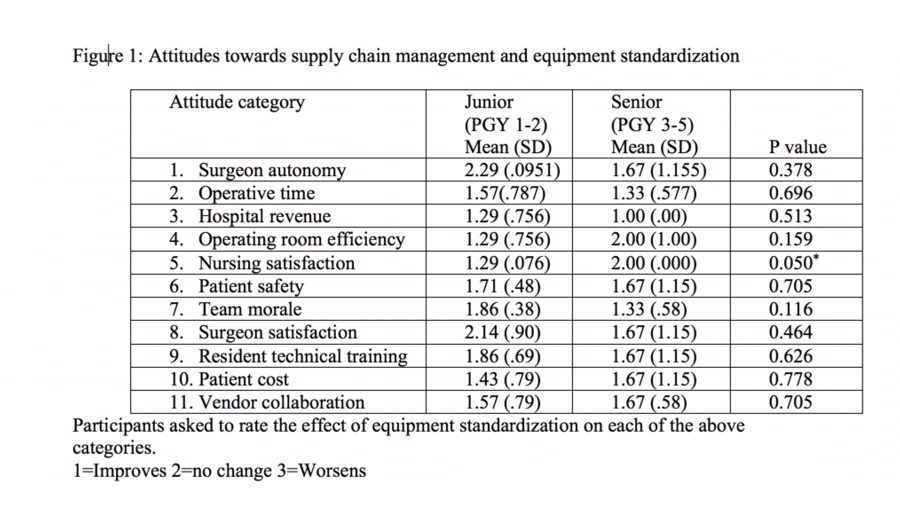
Methods: A multidisciplinary, interactive session was designed at a tertiary, academic medical center to address systems-based practice and specifically cost consciousness. As part of a quality improvement initiative, surgery residents participated in an hour-long mixed curriculum consisting of brief didactics and small group exercises. Participants were asked to develop an equipment standardization plan for laparoscopic appendectomy and cholecystectomy (common general surgical procedures) while assuming the role of department leadership. Supply management nursing provided all available instruments and prices were attached to each instrument. Each group then presented their standardization choices along with justification to the entire group. Faculty-led discussion addressed the challenges of balancing cost, effectiveness, and patient safety. Participants also completed surveys to assess their attitudes towards equipment standardization; residents rated their perception of and attitude toward 11 categories considered barriers to implementation of equipment standardization as “improves, no change, or worsens”. Mann Whitney U test was utilized to compare junior versus senior resident attitudes.
Results: Fifteen general surgery residents participated in the curriculum. There were 4 seniors (PGY 3-5) and 11 junior (PGY 1-2) residents. In general, participants felt that standardization improves or does not change metrics including surgeon autonomy, resident training experience, and patient safety (Figure 1). There was no difference between junior and senior residents with one exception, senior residents did not feel that OR nursing satisfaction changes whereas junior residents felt nursing were more satisfied.
Conclusion: Cost consciousness is an important aspect of systems-based practice for surgical residents. Our pilot curriculum addresses a gap in resident education about surgical cost. Residents generally regard equipment standardization as either improving or not changing hospital metrics.