PS2-02: A PROSPECTIVE, RANDOMIZED COMPARATIVE EFFECTIVENESS TRIAL OF TWO METHODS OF MIDTERM STUDENT PERFORMANCE FEEDBACK ON THE SURGICAL CLERKSHIP
David D Odell, MD, MMSc, Nabil Issa, MD, Trevor Barnum, RN, DNP, Jason Burke, BA, Susan Santacaterina, RN, Patricja Domanski, RN, Jonathan Fryer, MD, Amy Halverson, MD, MEd; Northwestern University Feinberg School of Medicine
Purpose: Feedback of performance to learners has long been recognized as an important instructional component in medical education. We sought to determine if in-person or written feedback on clinical performance resulted in more positive student performance on the surgery clerkship at our institution.
Methods: We developed two platforms for performance feedback to students: (1) one-on-one meetings between students and clerkship faculty and (2) detailed written performance feedback reports. Students enrolled in the surgery clerkship at our institution were block randomized by rotation in an alternating fashion to receive feedback at the mid-point of the 8-week surgical clerkship via either in-person or written communication. We then compared the performance of students in each group on the National Board of Medical Examiners (NBME) Surgery subject Shelf examination, formal end of rotation OSCE examinations, and clinical performance evaluations (CPE) received for each student at the completion of their clinical rotation. Composite performance evaluation for the clerkship served as the primary endpoint for the study.
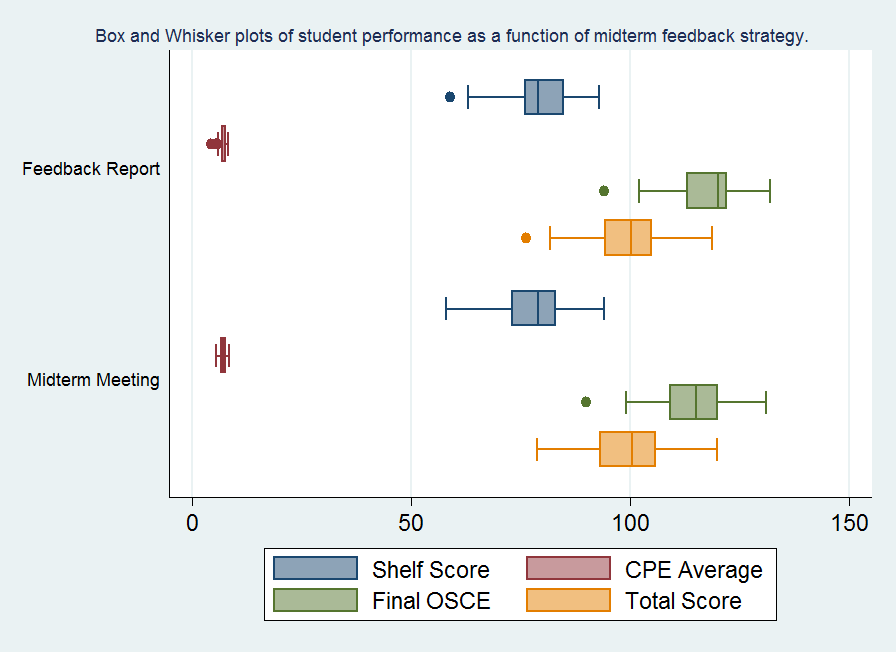
Results: A total of 146 students (6 rotations) participated in the study over a 12 month period. In-person feedback was given to 71 students and 75 received written feedback. Receipt of meaningful feedback was recognized by 97% of students in both groups on exit interviews at completion of the clerkship. No significant differences were seen between groups in NBME Surgery subject examination performance (p=0.35), clinical performance evaluations final OSCE examination score (p=0.94), or final clerkship rotation score (p=0.97). Performance on the final OSCE examination was significantly better for those students receiving written feedback (mean score 117.8 v. 114.5; p=0.01). When specifically assessing students at risk for failure based upon poor midterm examination or clinical performance, no difference was seen in performance on the NBME (p=0.89); final OSCE (p=0.14); CPE (p=0.27); or final clerkship grade (p=0.54).
Conclusions: Providing students with feedback on their performance is an important formative component of their clinical education. Written performance feedback reports demonstrated similar efficacy to traditional in-person feedback sessions in our study and may result in less disruption of clinical workflow for both students and faculty.
