PS2-09: SERVICE THROUGH SURGERY: THE IMPACT OF A SEMINAR COURSE ON MENTORSHIP AND STUDENT ATTITUDES ABOUT SURGERY, DIVERSITY, AND CARE FOR THE UNDERSERVED
Anna L Carroll, BA, Tyler S Bryant, MHS, Jecca Rhea Steinberg, MSc, Paloma Marin-Nevarez, BA, Sylvia Bereknyei Merrell, DrPH, MS, James N Lau, MD, MHPE, FACS; Stanford University School of Medicine
Introduction: Increasing diversity among surgeons improves healthcare outcomes for disenfranchised communities, but surgery continues to trail behind other specialties in racial, socioeconomic, and gender diversity. Mentorship is key in increasing surgical workforce diversity. We designed and evaluated a course that provided students with mentorship opportunities and exposure to diverse surgeons committed to addressing health disparities.
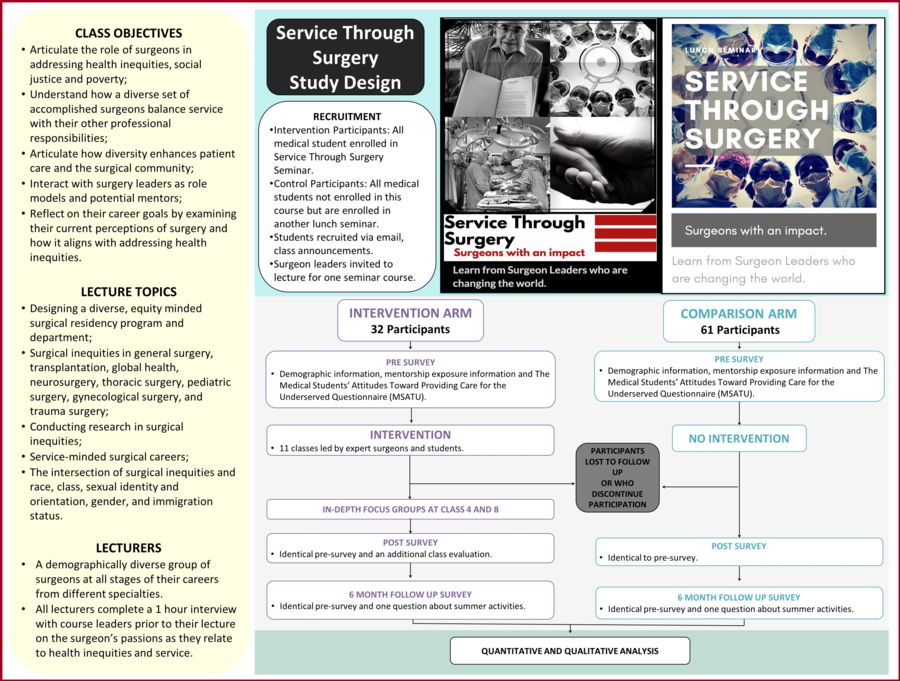
Methods: Service-minded surgeons of diverse races, genders, and sexual orientations lectured in a seminar series for medical students: “Service Through Surgery: Surgeons with an Impact.” We used survey tools with validity evidence to measure students’ attitudes towards surgical inequities, mentorship exposure, and demographic factors. We compared course participants’ (intervention) and non-participants’ (comparison) demographics using Chi-squared tests for variance and assessed attitudinal pre-post differences with paired t-tests, as well as independent t-tests for comparison of exposure changes between the intervention and comparison groups.
Results: A total of 93 students participated in the quasi-experimental study between January 2018-August 2018, with 32 intervention (53% women) and 61 comparison (59% women) participants, with over 25% representing disadvantaged backgrounds. Intervention participants were 40.6% white, 46.9% Asian, 6.3% Latinx, 3.1% multiracial. The intervention and comparison group demographics were similar (p>0.05) but varied in interest in a surgical specialty (intervention: 65.6%; comparison: 45.2%; p=0.01). There was a significant increase among intervention students newly meeting a surgeon of their race (intervention: 100%; comparison: 16.6%; p=0.004). There was a nonsignificant increase among intervention students newly finding a surgeon whose career they would like to emulate (p=0.224). There was a significant increase in the degree to which students expressed feeling personally responsible for providing surgical care to the needy (p=0.039), but not in the comparison group (p=0.80). Most participants (92.3%) indicated that they would recommend the class to other students.
Conclusions: Exposing medical students to diverse, service-minded surgeons through seminars like “Service Through Surgery” may make them more inclined to pursue such careers themselves. The class represents a replicable model for increasing mentorship in this space. A second iteration will take place in winter 2019.