PS5-02: IS CULTURE REALLY LOCAL OR ARE SURGICAL RESIDENTS A CONDUIT TO HARMONIZE BEST PRACTICES ACROSS DISTINCT DELIVERY SYSTEMS?
Tasce Bongiovanni, MD, MPP, Elizabeth Lancaster, MD, Joseph Lin, MD, Kristin Slown, PharmD, Keith Hansen, MD, Pat O'Sullivan, EdD, Elizabeth Wick, MD, Kenzo Hirose, MD; UCSF
Introduction: For many patients, opioid addiction begins with exposure at time of surgery. At teaching institutions, surgical residents are often prescribers, with variable oversight from attending physicians. Quality can be improved by increasing adherence to evidence-based practices, usually at the hospital or health system level. However, many surgical residency programs comprise multiple delivery systems. We hypothesized that surgical residency-based intervention addressing opioid prescribing will improve care and will change residents prescribing patterns by increasing the percentage of patients discharged with non-narcotic analgesic medication (acetaminophen and ibuprofen) in an especially vulnerable population at our urban trauma center.
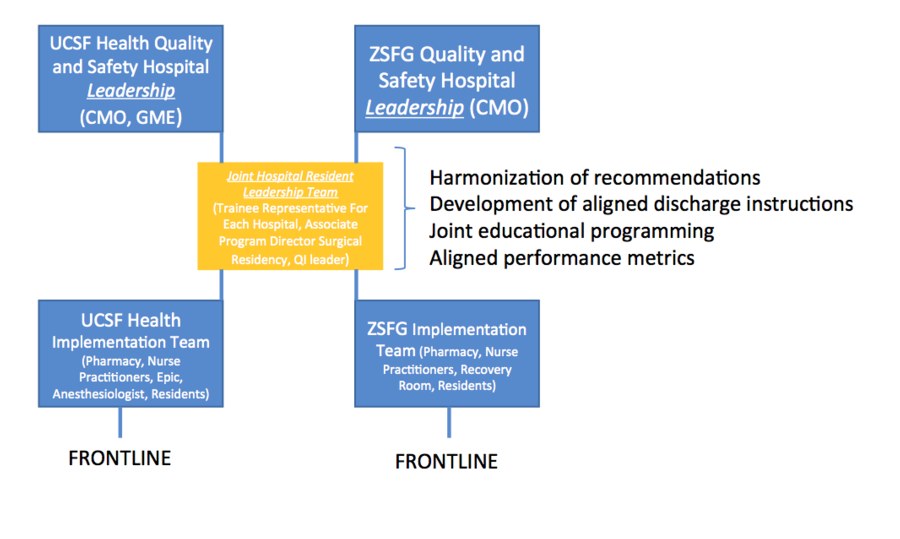
Methods: We designed a multi-faceted resident led intervention to ensure that standard evidence based analgesia prescribing was occurring at a large academic medical center as well as public safety net hospital, both essential education sites for the residency program but with distinct leadership and faculty. The intervention included a collaborative resident leadership model with representation from each site and used the same combination of didactics, local transdisciplinary improvement teams and performance feedback at both sites.
Results: First, we came to consensus on included surgical procedures, discharge pain recommendations for residents as well as discharge pain instructions for the patients across the multiple sites. Then, we began capturing data, which we used to provide feedback to residents on a monthly basis. We captured a total of 42 general surgery cases in our pilot study period, 22 in the pre-intervention period, 20 in the post-intervention period. Pre-intervention, 82% of patients were discharged on narcotics, 45% were discharged on acetaminophen, and only 5% were discharged on ibuprofen. In the post-intervention period, 67% of patients were discharged on narcotics. Importantly, 81% of patients were discharged on acetaminophen, and 71% were discharged on ibuprofen.
Analysis: This novel model of a residency-based improvement program addresses both the complexity that trainees in multisite programs face in understanding local culture at each hospital and also demonstrates that residents can be effective at accelerating change. This is particularly important at safety net hospitals, where hospital quality improvement and information technology resources are more limited, but where improvement work is perhaps even more essential.