PS5-08: THE IMPACT OF RESIDENT INVOLVEMENT ON OUTCOMES IN BREAST CANCER SURGERY
Austin D Williams, MD, MSEd, Robin M Ciocca, DO, Barry D Mann, MD; Lankenau Medical Center
Introduction. Perceptions about the impact of intraoperative resident involvement on surgical outcomes are often negative, but the literature presents mixed results. Breast cancer surgery is an important competency for general surgeons, so resident exposure is important, but its impact on patient morbidity is unknown.
Methods. We queried the American College of Surgeons National Surgical Quality Improvement Program database for patients undergoing lumpectomy, lumpectomy with axillary sampling, simple or subcutaneous mastectomy or modified radical mastectomy during the years 2007-2012. We grouped patients by whether a resident was involved in the case and further stratified by post-graduate year (PGY). For each surgery type, we compared operative time, the rates of >15 postoperative morbidities and the rates of unplanned 30-day readmission and reoperation with univariate and multivariate analyses.
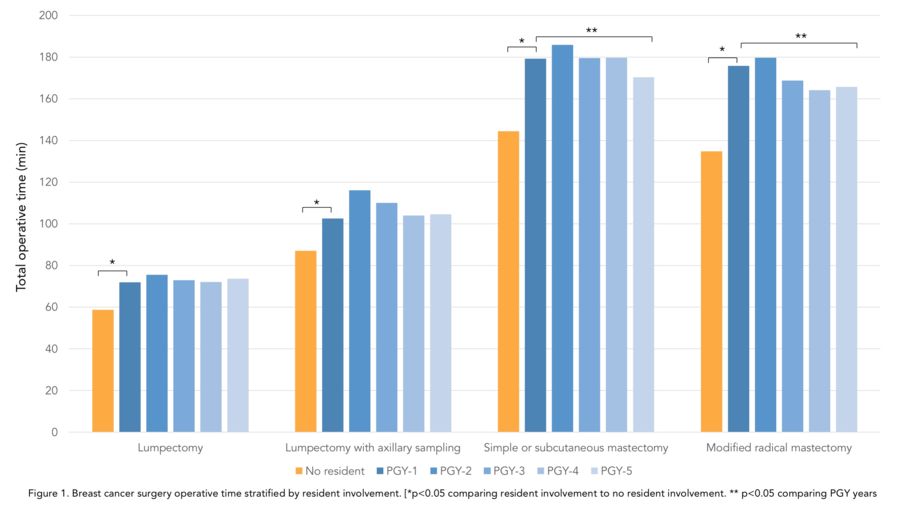
Results. Resident participation was documented in 54.3% of the 66,061 included cases. PGY-1, 2 and 3 residents assisted in the largest proportion (72.1%) of these cases. There were no differences in preoperative estimated risk of mortality for patients between patients undergoing surgery with or without resident involvement (p>0.05). Cases in which residents were involved had a significantly longer total operative time, and mastectomy cases were significantly longer if a junior resident was involved (Figure 1). Surgeries involving PGY-2 residents had the longest operative time for all surgery types (p<0.01). There were few differences in the rates of medical comorbidities when comparing patients undergoing surgery with or without resident involvement. In the lumpectomy group, resident involvement was associated with a higher incidence of superficial site infections (1.26 vs. 0.95%, p=0.02). Resident involvement was also associated with bleeding requiring transfusion in both simple or subcutaneous (0.88 v. 0.52%, p=0.004) and modified radical mastectomy (0.97 v. 0.72%, p=0.003) groups. There were no differences in the rates of unplanned reoperation and readmission (p>0.05).
Conclusions. Resident involvement is associated with increased operative time in breast cancer surgery, which is required to allow for teaching and to permit some level of operative autonomy. While there are also some associations with infection and bleeding risk, resident involvement does not appear to contribute considerably to overall patient morbidity.