PS8-05: MAKING CENTRAL LINES SAFER: A MULTIDISCIPLINARY PROGRAM TO IMPROVE OUTCOMES FOR RESIDENT-PERFORMED ULTRASOUND GUIDED CENTRAL VENOUS ACCESS
Bao-Ling Adam, PhD, Richard Gordon, MD, Steve Holsten, MD, Matthew Lyon, MD; Medical College of Georgia at Augusta University
Objectives: The “Making Central Lines SAFER” initiative is a comprehensive program to decrease complications, both mechanical and infectious, from resident-performed ultrasound guided central venous access (USGCVA). This program was implemented to address the need for a standardized USGCVA technique, Graduate Medical Education (GME) inter-specialty training, and interdisciplinary competency testing for USGCVA.
Methods: A training course composed of didactic lectures on asepsis techniques, complications, principles of ultrasound guidance, and institutional standards for catheter placement was implemented and delivered to the residents. The competency testing was then completed by each participant using a novel ultrasound-gel based cadaver model utilizing either the internal jugular, subclavian, or femoral vein with faculty supervision using a standardized grading rubric. Based on performance, residents were assigned a pass or fail grade. Only central venous lines placed by residents in adult patients and central line-associated blood stream infections (CLABSI) occurring within 7 days of insertion were included in the analysis. CLABSI data pre and post the training was collected from institution epidemiological monitoring. CLABSI rates were calculated in per thousand central line days for each quarter using hospital-wide data.
Results: In 2016/2017 academic year, 214 residents completed the training and took the performance based assessment. 32% (n=72) did not pass the USGCVA competency assessment. The median resident CLABSI rate before training was 0.3755/1000 days. The median CLABSI rate after training was 0.1448/1000 days (p value 0.2857). These values included all resident regardless of assessment outcome. When residents who failed the competency assessment were removed from the post training analysis the CLABSI rate was 0.00 (p value 0.0238). In 2017/2018 academic year, 67 new interns completed the training and took the performance based assessment. 55.2 % (n=37) of participating residents passed the USGCVA Competency Test. The number of CLABSIs was significantly reduced after the USGCVA Competency Testing in September 2017. See Figure 1.
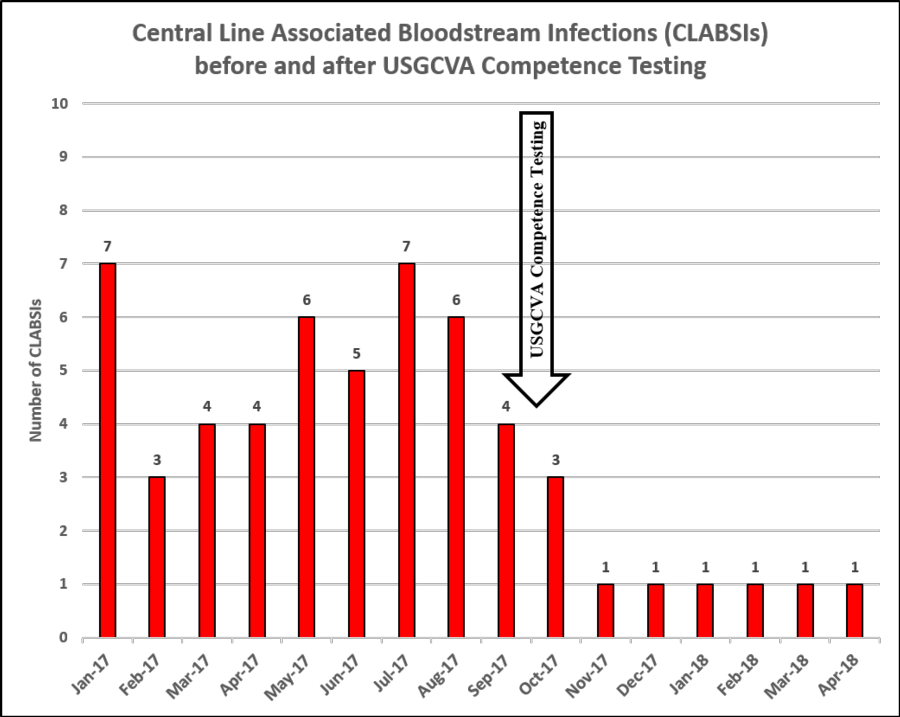
Conclusion: After only two years of implementation, the Making Central Lines SAFER program has eliminated major procedural complications and drastically reducing CLABSI. This program has successfully standardized the techniques, equipment, training, and competency testing for USGCVA, decreasing patient complications, and saving the health system financial resources.
