PS9-04: OPERATIVE PERFORMANCE OUTCOMES OF A SIMULATOR BASED ROBOTIC SURGICAL SKILLS CURRICULUM
William Gerull, Ahmed Zihni, MD, MPH, Michael Awad, MD, PhD; Washington University in St. Louis School of Medicine
Background: Robotic technology has become increasingly prevalent throughout modern surgical practice, as surgical training programs are determining how to best include this training in their curricula. Previously described curricula have detailed robotic skills enhancement in a laboratory setting. In this study, we sought to measure changes in performance and workload metrics in the live operative setting following the completion of a novel simulator-based robotic skills curriculum.
Methods: 31 residents from general surgery, urology, and gynecology naïve to robotic platforms were recruited in this IRB-approved study. Subjects participated in a live robotic case and had a baseline assessment using RO-SCORE, a robotic modification of the O-SCORE tool, and self-assessed their workload using the NASA Task Load Index (NTLX). Subjects then completed the curriculum, created by an expert panel, on a daVinci Skills Simulator (dVSS) to pre-set proficiency goals. Trainees were encouraged to come on their own time and could complete the curriculum in one or more sittings, in a 1 week time period. Subjects were then assessed after another live case. Data were analyzed using paired student’s t-test.
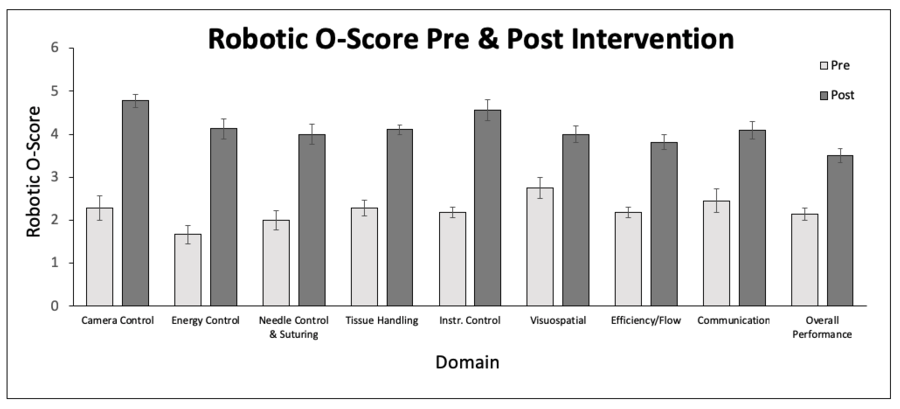
Results: Completion of the curriculum required an average of 2.3 hours and was associated with significant RO-SCORE improvements in operative performance across all domains including camera control (2.2 pre, 4.9 post, 95% CI: 1.57-3.22), needle control (1.9 pre, 4.1 post, 95% CI: 1.10-2.54), tissue handling (2.3 pre, 4.4 post, 95% CI: 1.45-2.20), and overall performance (2.2 pre, 4.5, 95% CI: 0.85-1.57). Significant reductions in NTLX workload ratings in Physical Demand (5.1 pre, 2.4 post, 95% CI: -3.51 - -1.26), Effort (6.9 pre, 3.4 post, 95% CI: -3.47 - -1.89), and Frustration (6.3 pre, 1.4 post, 95% CI: -5.38 - -3.70) were also seen.
Conclusions: We describe a feasible robotic simulation curriculum that requires a reasonable amount of time for surgical trainees and, importantly, is self-directed. Significant improvements were seen across the board in all performance metrics and subjective operator workload. Importantly, this translated to the clinical environment. These types of curricula will be necessary for improving the skills and confidence of both trainees and attending surgeons alike as robotic technology becomes more pervasive.