Plenary1-01: CAN DISCOURSE ANALYSIS PREDICT SURGICAL OUTCOMES? EVALUATING HOW WE TALK IN THE OPERATING ROOM AND WHAT IT MEANS.
Anne-Lise D D'Angelo1, Andrew Ruis2, David W Shaffer3, Carla M Pugh4; 1Mayo Clinic-Rochester, Department of Surgery, 2University of Wisconsin-Madison, Wisconsin Center for Education Research, 3University of Wisconsin-Madison, School of Education, Department of Educational Psychology, 4Stanford University, Department of Surgery
Introduction: Communication in the operating room has largely been studied in the context of surgical leadership and situation awareness. Our hypothesis is that qualitative discourse (speech) analysis can be used to distinguish procedural outcomes during a simulated procedure.
Methods: Audio recordings of senior residents at a national meeting (N=11) were captured while performing a simulated laparoscopic ventral hernia (LVH) repair.
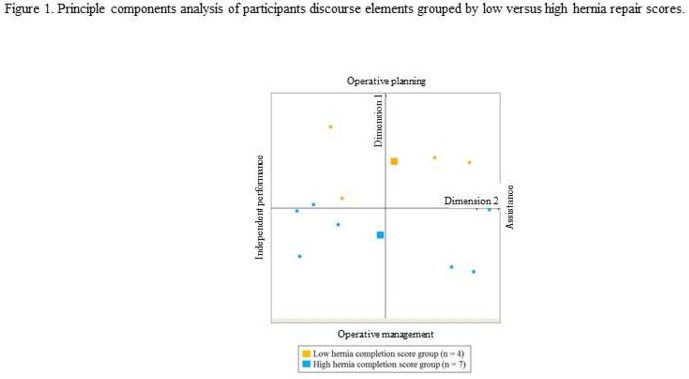
Using an iterative process grounded in qualitative analysis, five discourse elements were generated (operative planning, identifying errors, asking for advice, giving assistant instruction and assistant giving advice) from the audio-recordings, and the transcripts were coded accordingly (κ>0.67). A computational software program, epistemic network analysis, was utilized to perform a principal components analysis on the connections between the discourse elements to generate dimensions of performance.
The LVH repairs were assessed for completeness using a 17-point rating scale (κ=.83). Hernia repair scores were used to separate participants into low and high performers.
Independent-samples t-tests were used to evaluate differences between the operative discourse of participants with low and high hernia repair scores.
Results: There was a significant difference between the mean hernia repair scores for the low performers (M=3.8/17; SD=.96) and the high performers (M=9.3/17; SD=2.8), t(9) = –3.74, p=.005.
Figure 1 illustrates the distinction between the operative discourse of residents with low versus high hernia repair scores. There was a significant difference in operative discourse on Dimension 2 (Operative planning vs Operative management). Participants with low hernia repair scores (M=.23, SD=.14) had greater connections between discourse elements operative planning and asking for advice (Operative planning), while participants with high hernia repair scores had greater connections between discourse elements giving assistant instruction and identifying errors (Operative management) (M= -.132; SD=.14), t (6.33)=4.02, p=.006. There was no significant difference in operative discourse between participants with low and high hernia repair scores on Dimension 1 (Independent performance vs Assistance) p=.78.
Conclusion: Participants with higher hernia repair scores engaged in more operative management communication during the simulated procedure. The ability to integrate and manage multiple operative steps and verbally communicate them represents higher-level decision making and significantly correlates with surgical outcomes.