Plenary1-02: DESIGN, IMPLEMENTATION AND LONG TERM FOLLOW-UP OF A CONTEXT SPECIFIC TRAUMA TRAINING COURSE IN UGANDA: LESSONS LEARNED AND FUTURE DIRECTIONS
Sarah Ullrich, MD1, Cathy Kilyewala, MBBS2, Michael Lipnick, MD3, Maija Cheung, MD1, Martha Namugga, MBBS2, Peter Muwanguzi, MBBS4, Michael DeWane, MD1, Arlene Muzira, MBBS4, Janat Tumukunde, MBBS4, Monica Kabagambe4, Naomi Kebba, MBBS4, Moses Galukande, MBBS2, Jacqueline Mabweijano, MBBS2, Doruk Ozgediz, MD, MSc1; 1Yale University Department of Surgery, 2Mulago Hospital Department of Surgery, 3University of California San Francisco Department of Anesthesia, 4Makerere University School of Medicine
Background: The Kampala Advanced Trauma Course (KATC) was developed in 2008 in response to a locally identified need for an advanced trauma training curriculum tailored to a resource-constrained setting. Existing courses were cost-prohibitive, did not fit the local context, or were intended for non-physician providers. Since its inception, the course has been taught to over 800 trainees. We describe the design of the course and report impact evaluation through a participant survey.
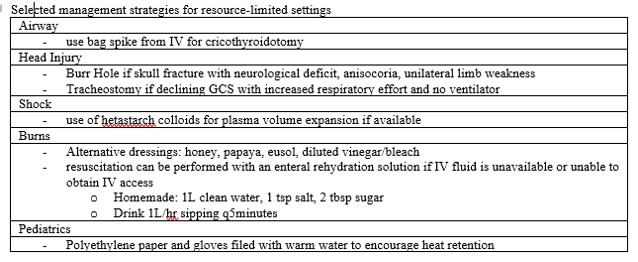
Methods: Context-appropriate didactic modules, skill stations, and exams were developed through local experts and international collaborators in 2008 and refined 2008-2012. Ugandan surgical faculty delivered the course. Questionnaires were designed, piloted, validated, and administered to KATC participants from 2013 – 2016 to identify confidence in performing and teaching various skills, challenges in delivering trauma care, and priority areas for additional trauma surgical training.
Results: Of 295 participants, 106 responded. After taking KATC, over 50% of respondents felt confident performing and teaching airway management, shock, burns, chest trauma, BLS, log rolling and c-spine management. Over 80% of participants were confident with all skills except venous cut-down. Participants rated airway management (30.2%) and shock (27.4%) as the most important skills. More support was needed for head trauma (26.4%) and venous cut down (19.8%). Lack of equipment (52.8%) and inadequate staffing (22.6%) were the most commonly identified barriers to providing care.
Conclusion: This is the most long-standing trauma course tailored to the resource-limited setting in the current literature. Respondents reported increased confidence in most essential skill sets for trauma care. Minimal dependence on instructors from high-income countries has allowed the course to be sustainable and has maximized local relevance. Course scale up is underway. Additional research is needed to more directly assess changes in practice patterns and clinical outcomes after formal trauma training.