Poster4-04: THE LINK BETWEEN INDIVIDUAL TECHNICAL ERROR AND ADVERSE PATIENT OUTCOME
Debolina Kanjilal, Fizza Mahmud, Gary Sutkin, MD; UMKC
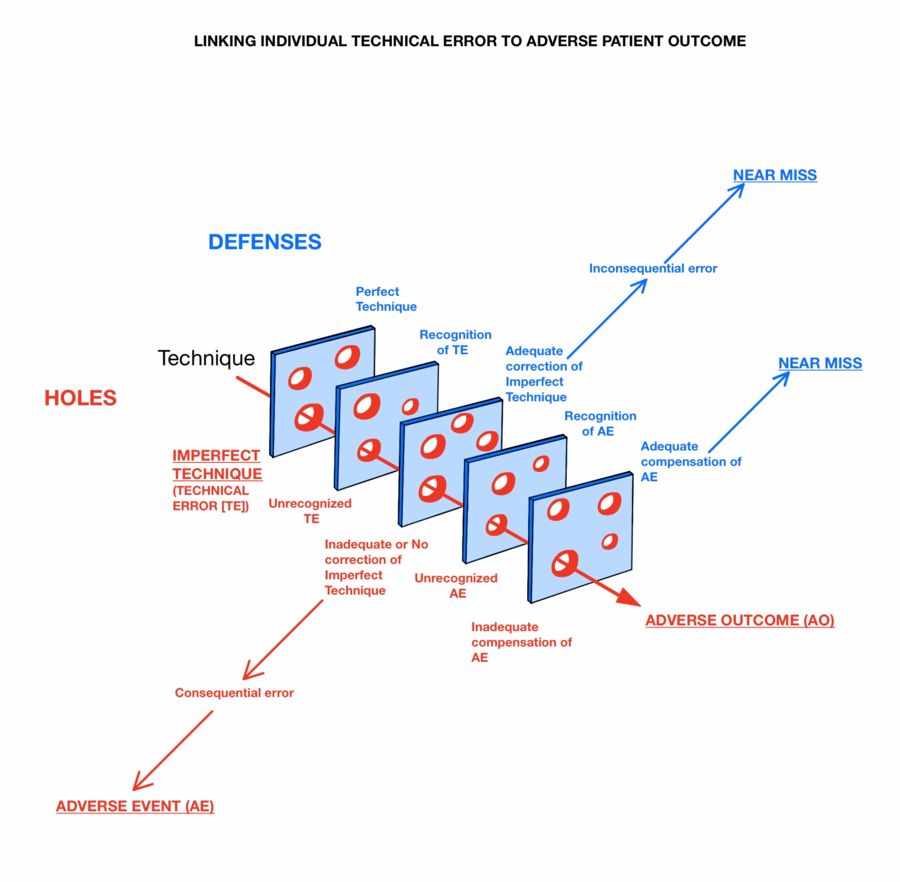
Methods: We used Constructivist Grounded Theory methodology, starting with a comprehensive review of the literature and interviews with three surgeons, focusing on avoidance of technical errors. This allowed us to develop an initial model, refine our semi-structured interview, and interview more surgeons. Both the model and our interview script were revised iteratively with each interview and further review of the literature. We were particularly influenced by B. Tang’s human reliability study of intraoperative errors, differentiating procedural and execution errors, and J.T. Reason’s Swiss Cheese model, illustrating how holes in defenses predispose patients to harm. Interviews ceased when data saturation was reached and the model no longer changed. We reviewed the updated model with earlier interviewed surgeons.
Results: The surgeons in our sample provided a broad range of technical errors linked to adverse events. Each error occurred during a high-risk step and was defined by a unique improper technical motion that without a compensatory response, would have led to one or more discreet adverse events. Our model (figure) accounts for technical errors, adverse events, and adverse outcomes. It includes five primary defenses against an adverse event, including perfect technique, recognizing imperfect technique, adequately correcting imperfect technique, recognizing an adverse event, and adequately compensating for an adverse event. Adequate compensation at the level of imperfect technique or at the level of an adverse event results in a near miss.
Conclusion: Our model links dichotomous surgical technique to adverse patient outcomes across multiple surgical specialties and can be used to prospectively study this association. The model is useful in teaching error prevention as an active process in surgery, rather than a latent one, by helping develop intra-operative strategies to prevent surgical errors.
