Poster4-05: A NOVEL BIOMEDICAL ENGINEERING-BASED SYSTEM TO ENHANCE LAPAROSCOPIC SURGICAL SIMULATION TRAINING USING BIOFEEDBACK
Brian M Sweis, PhD, Jillian V Schommer, BS, Joseph R Slaughter, BS, Andrew Cleland, MD, Jonathan Schrope, BS, Caleb Fick, Tanner McArdle, Victor Vakayil, James V Harmon, MD, PhD; University of Minnesota
Background: Technical proficiency is critical to laparoscopic skills training. While most simulators focus on procedural competency, less emphasis is placed on the appropriate tissue handling. Intraoperative variables such as torque, direct force, and trocar insertion angle are critical to avoid intra-abdominal injury. Proper surgical technique mandates atraumatic tissue manipulation; incorporating technology that provides real-time, biofeedback-based training, may enhance simulation and surgical learning. This technology is not yet widely available in laparoscopic surgical simulators.
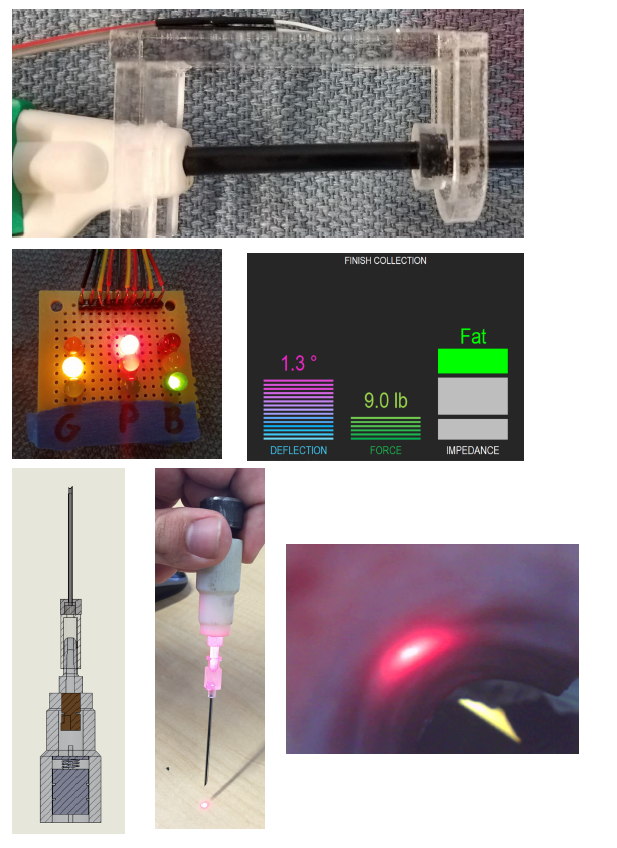
Methods: Three teams of biomedical engineering students at the University of Minnesota worked directly with our surgical education team to design novel smart-instruments to enhance laparoscopic simulations. Three tools were developed to teach surgical skills including: (1) torque and pressure control, (2) delicate tissue handling and grasp-strength, and (3) percutaneous abdominal access with accurate needle placement. These smart-instruments were designed to provide enhanced real-time physiological feedback to the user during surgical training. Each instrument was individually calibrated to provide standardized performance metrics.
Results: A “smart trocar” was developed to provide biofeedback on the torque and pressure delivered to tissue at the port site. The angle of incidence, applied force, and impedance-determined tissue type at the tip of the trocar is displayed on screen in real time. “Smart forceps” provide biofeedback on tensile force applied to tissues. Force and position are measured with a sensor in the forceps using a strain gauge load-cell and transmitted to a digital display on the tool itself. A “smart percutaneous needle” provided laser-guided tissue visualization to improve puncture site localization and angle of entry during advancement of the finder needle.
Discussion: Existing surgical simulations familiarize trainees with the basics of instrument handling, however proficiency in delicate tissue handling is otherwise only acquired through trial-and-error practice in the OR. Combining multiple smart-instruments into a single surgical simulation laboratory skills suite, surgical training centers can develop robust teaching curricula based on biofeedback approaches that facilitate skill enhancement through self-calibration by the learner in real time.